Endometritis vs. Endometriosis: What Is The Difference?

By Halle Tecco, MBA, MPH
In a world where medical terminology can be overwhelming, clarity is important—especially when it comes to conditions affecting the uterus. Two conditions, endometriosis and endometritis, frequently fall victim to mix-up. Despite the similarity in names, these conditions are distinct both in terms of origin and impact. In this article, we will break down the differences and similarities between these two conditions, providing you with a clear roadmap for understanding.
To the layperson—or even the medical professional—these two conditions may present as medical doppelgängers, due to their overlapping symptoms. So before diving into the distinct nature of endometriosis and endometritis, let’s talk about exactly what they are.
What Is Endometriosis?
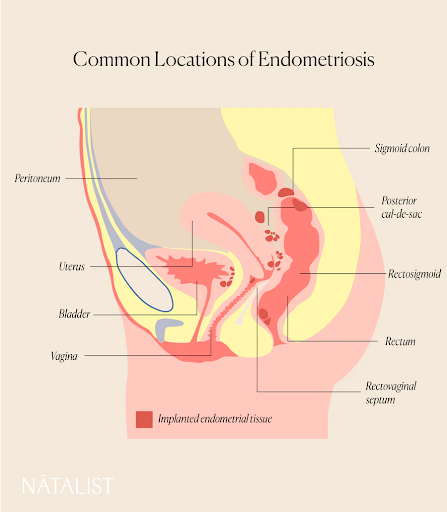
Endometriosis manifests when tissue resembling endometrial cells, which normally line the uterus, grows outside of the uterus. [1] Often, these extraneous cells encroach upon the ovaries, fallopian tubes, and even the bladder and bowel. The cause of endometriosis is unknown. [1]
Symptoms and conditions associated with endometriosis may include [1]:
- Severe pelvic pain, especially during menstrual periods
- Pain during sex or when using the bathroom
- Heavy bleeding during or between periods
- Gastrointestinal symptoms like bloating, diarrhea, or constipation
- Fatigue
- Nausea
- Depression or anxiety
- Infertility
Learn more about what endometriosis feels like →
What Is Endometritis?
Endometritis, at its core, is an inflammation of the endometrium—the inner lining of the uterus. [2] There are two types of endometritis: acute and chronic. Acute endometritis inflammation typically stems from infection, which may be due to complications from childbirth, miscarriage, sexually transmitted infections (STIs), or certain medical procedures like dilation and curettage (D&C). [2] Chronic endometritis, which is continuous, mild, and harder to diagnose, is most commonly caused by chronic bacterial infection. [2-4]
Symptoms and conditions associated with endometritis may include [2]:
- Fever
- Irregular or heavy bleeding
- Lower abdominal pain
- Recurrent pregnancy loss
- Repeated implantation failure
- Infertility
Endometritis vs. Endometriosis
Endometriosis is very common, and is estimated to affect more than 11% of women between 15 and 44, being especially common among women in their 30s and 40s. [3] The prevalence of endometritis is a little harder to pin down; estimates range from 0.2% to 46% for chronic endometritis. [4]
Both conditions manifest in pelvic discomfort and can even coexist. [3-4] Since there is a lot of overlap in symptoms, it can be difficult to determine if you have endometriosis or endometritis without seeing a provider.
Here is how medical providers generally differentiate between the two:
Clinical Evaluation
Your healthcare provider will likely want to review your medical history, perform a physical exam including a pelvic exam, and get tissue samples for lab tests. [4] For endometritis, they may take a swab culture from the cervix or look at vaginal discharge samples under a microscope. [4] For endometriosis, the majority of healthcare providers will diagnose endometriosis using laparoscopy, an operation that allows the provider to examine internal organs. Providers may also examine tissue under a microscope. [3]
Blood Tests
Blood tests are generally more useful for ruling out other conditions (like pelvic inflammatory disease, or PID) than for definitively diagnosing either endometriosis or endometritis. For instance, an elevated total leucocyte (white blood cell) count might suggest infection and lend support to a diagnosis of endometritis. [4] Unfortunately, there is currently no specific blood test to diagnose endometriosis (although researchers are working on this!). [1,3,5]
Imaging
Transvaginal ultrasounds may be performed to help diagnose or monitor either condition. For endometritis, your providers will be looking for a thickened endometrial lining or fluid in the uterus – signs of inflammation. [4] For endometriosis, they will be looking for ovarian cysts from endometriosis. [3] A clinician might also order an MRI (magnetic resonance imaging) to get a better look at your reproductive organs. [3]
Surgery
Ultrasounds often fall short of definitively diagnosing endometriosis. For a concrete diagnosis, laparoscopy is generally employed. This surgical procedure involves inserting a camera into the pelvic area to search for the extraneous endometrial-like tissue. [3] Read more about laparoscopy for endometriosis.
Can You Have Both Endometriosis and Endometritis?
Yes, you can have both endometriosis and endometritis. In fact, one study found that more than half of endometriosis patients also had chronic endometritis, noting a strong association between the two. [5] However, the authors noted that the cause of chronic endometritis in endometriosis is still unclear. It could be an infection or from the endometriosis itself. [5]
Endometriosis, Endometritis, and Infertility
Unfortunately, both endometriosis and endometritis are linked to infertility. Each condition, with its unique pathology, carries distinct implications for fertility. Some facts:
- 25 to 50% of infertile women have endometriosis [6]
- 30 to 50% of women with endometriosis are infertile [6]
- 45% of infertile patients have chronic endometritis [4]
Endometriosis is thought to impair fertility in several ways, including altered anatomy due to adhesions, altered pelvic environment leading to poor egg or sperm transport, and inflammatory changes that may affect fertilization and implantation. [4,6] However, it's worth noting that many women with endometriosis can conceive unassisted or through IVF (in vitro fertilization). [1,3,6]
The connection between endometritis and infertility has received less attention. However, we know that chronic endometritis has been associated with recurrent pregnancy loss and implantation failure during in vitro fertilization (IVF) treatments. [4] One thought is that the inflammatory nature of endometritis could interfere with the endometrial receptivity needed for a fertilized egg to implant in the uterine lining. [4] Once diagnosed, however, antibiotic treatment of endometritis often resolves the inflammation, and fertility may be restored, although more studies are needed to understand the long-term implications fully. [4]
Summing It Up
Endometriosis and endometritis, though entangled by both name and symptom similarities, are uniquely challenging—especially concerning fertility.
What is clear is that education and awareness are critical. Understanding the nuanced differences between the two conditions can help steer you towards more tailored, effective healthcare. Indeed, there are critical gaps in our understanding of how these conditions interact, especially when they co-exist. However, ongoing research and patient advocacy may one day lead us to fill these gaps.
If you are suffering through any of the symptoms listed above, the first step is consultation with a healthcare provider experienced in reproductive health. No webpage, article, or diagnostic quiz can replace the expertise that comes from a comprehensive medical evaluation. (Although I hope this article gave you the distinctions you ought to know, as you advocate for your health).
So, while researchers continue to unravel the mysteries of these conditions, you, too, have a role to play: that of an informed, proactive patient. It can be a frustrating journey, but not one you have to make alone. We wish you all the best! If you are on a fertility journey, speak to your provider about what fertility products and supplements may benefit you. From fertility tests to high-quality vitamins, Natalist has got you covered.
Read more:
- Getting Pregnant with Endometriosis
- Endometriosis Risk Factors: An Overview
- Is Endometriosis an Autoimmune Disease?
References:
- Endometriosis. World Health Organization. Accessed October 2023. URL.
- Taylor M, Jenkins SM, Pillarisetty LS. Endometritis. [Updated 2023 Feb 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. URL.
- Endometriosis. Office of Women’s Health. U.S. Department of Health & Human Services. Accessed October 2023. URL.
- Singh N, Sethi A. Endometritis - Diagnosis,Treatment and its impact on fertility - A Scoping Review. JBRA Assist Reprod. 2022;26(3):538-546. Published 2022 Aug 4. doi:10.5935/1518-0557.20220015
- Takebayashi A, Kimura F, Kishi Y, et al. The association between endometriosis and chronic endometritis. PLoS One. 2014;9(2):e88354. Published 2014 Feb 18. doi:10.1371/journal.pone.0088354
- Bulletti C, Coccia ME, Battistoni S, Borini A. Endometriosis and infertility. J Assist Reprod Genet. 2010;27(8):441-447. doi:10.1007/s10815-010-9436-1
Reach Out, We're Here
Have questions about your order or products? For the speediest answer, check out our FAQ section. Need something else? Come find us below.
Please keep in mind our regular business hours; Monday-Friday, 9am-5pm CT.
Customer Support
support@natalist.com
Press Inquiries
media@everlyhealth.com
Business & Partnerships
team@natalist.com
Affiliates + Influencers
team@natalist.com
Job Openings
Careers Page

























