What's a Good AMH Level at Every Age?

Originally published 08/04/2021. Updated for accuracy and relevancy on 02/18/2024
By OBGYN and fertility expert Dr. Kenosha Gleaton
You may have heard about one of the most popular hormones on the block, AMH (short for anti-müllerian hormone). Perhaps you even got AMH testing done at your clinic, or at home. In this guide, we’ll review what this hormone can (and can’t) tell you and share the latest research on the topic.
What Is AMH?
AMH is a hormone expressed by granulosa cells of the ovary during a woman’s reproductive years. A gradual increase in AMH levels is observed in girls from the first day of life, with maximum levels observed in women at around the age of 25.1 In adult women, AMH decline occurs as the primordial follicle pool declines with age, becoming undetectable at menopause.
What AMH Can’t Tell You
There is no single test that can tell you with certainty your likelihood of getting pregnant.
To understand ovarian reserve (the reproductive potential based on egg count and quality), a number of screenings may be utilized, but no single test is highly reliable for predicting pregnancy potential. In addition to AMH testing, your doctor will likely look at day 3 FSH, day 3 estradiol, antral follicle count, and more.
No single test is highly reliable for predicting pregnancy potential.
Multiple studies show that AMH doesn’t correlate with how likely you are to get pregnant.2,3 Getting pregnant depends on many different factors, and AMH does not assess egg quality, the quality of the ovaries, sperm quality, or the health of the womb.
One study tracked 981 women aged 30 to 44 years.4 The women had their ovarian reserve tested using three hormones (AMH, FSH, and inhibin B) and were followed for a year. The study showed that there was no correlation between a woman’s ovarian reserve and her ability to conceive, and that a low ovarian reserve was not associated with reduced fertility level.4 The researchers concluded: "These findings do not support the use of urinary or blood FSH tests or AMH levels to assess natural fertility..."
What AMH Can Tell You
For women undergoing IVF (in vitro fertilization) treatment, research shows that AMH levels correlate with the number of oocytes (eggs) retrieved after stimulation and can help predict ovarian response.7 However, while AMH has some association with predicting live birth after IVF treatment, its ability to predict live birth is poor.5
So what is a good AMH level for IVF ? One study suggested the following general guidelines for AMH value and IVF4:
- AMH <0.5 ng/mL predicts difficulty in IVF getting more than three follicles to grow, which in turn reduces the chance of pregnancy with IVF.
- AMH <1.0 ng/mL suggests a limited egg supply, and a short window of opportunity to conceive.
- AMH >1.0 ng/mL but <3.5 ng/mL suggests a good response to IVF stimulation.
- AMH >3.5 ng/mL indicates an ample and healthy egg supply, and suggests caution should be exercised in order to avoid ovarian hyperstimulation syndrome (OHSS).
An AMH test is also a strong predictor for the timing of menopause. Research shows that low AMH levels occur approximately five years before menopause.1 Other research indicates that the time of menopause may be predicted via a mathematical model on the basis of a single AMH measurement and the age of the patient.
What Is a Good AMH Level?
For every woman, AMH levels by age will decrease and there’s not a lot we can do about that.6 However, I encourage you not to stress about your AMH level! As stated earlier, AMH is just one measurement your doctor looks at to assess overall ovarian reserve. Your AMH result is not predictive of your chances of conceiving naturally, and certainly does not define your fertility.
In general, a normal AMH level for a woman of reproductive age is 1.0–4.0 ng/ml.
Median AMH Levels at Every Age
One study looked at the median AMH levels (ng/mL) in 2,741 women4:
- Under 25 = 5.13
- 25 = 5.42
- 26 = 4.91
- 27 = 4.12
- 28 = 4.96
- 29 = 3.87
- 30 = 3.53
- 31 = 3.59
- 32 = 3.44
- 33 = 2.70
- 34 = 2.49
- 35 = 2.58
- 36 = 2.28
- 37 - 1.85
- 38 = 1.66
- 39 = 1.72
- 40 = 1.27
- 41 = 1.26
- 42 = 1.20
- 43 = 0.81
- >43 = 0.72
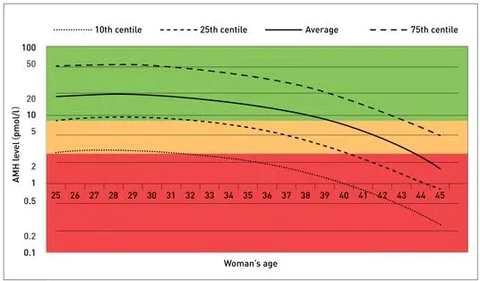
The following chart shows the average AMH (in pmol/l) for women by age. Please note: this table should not be compared to the numbers above (in ng/mL) as they are measured in different increments.
How Can I Increase My AMH?
I am often asked how to increase AMH levels. While there are no definitively proven ways to achieve higher AMH levels, there are ways to increase your chances of getting pregnant.
Can AMH Go Up and Down Month Over Month?
In general, AMH is considered a stable hormone that doesn’t fluctuate greatly month over month. However, according to studies on AMH fluctuations, young women can experience both low AMH levels and higher AMH levels.3 The studies report that symptoms of low AMH levels were observed during the very early luteal phase, directly after ovulation for young women.3 However, for older women, the range of AMH level fluctuation over a menstrual cycle was very low.
Beware of Comparing Your AMH Level to Others
Because there is no international standard for AMH levels, the interpretation of AMH levels is laboratory assay-dependent, meaning it can vary from lab to lab and test to test. Your clinician should give you the laboratory's reference ranges. If you have an AMH test in one lab one year, and another the next, talk to your doctor before comparing the test results to ensure it’s apples to apples.
Be Informed, But Don’t Over Worry
For every woman, AMH levels will decrease with age and there’s nothing we can do about that. I encourage you not to stress if you have low levels!3 AMH is just one measurement your doctor looks at to assess overall ovarian reserve. Your AMH result is not predictive of your chances of conceiving naturally, and certainly does not define your fertility.
At Natalist, we’re here to support you every step of the way as you embark on this journey with resources like our women’s prenatal vitamins with folate to support your body’s nutritional needs and our early detection pregnancy test for timely insights into your pregnancy!
Dr. Kenosha Gleaton is board-certified in gynecology and obstetrics and is the Medical Advisor of Natalist. She received her MD from MUSC and completed her residency at Carolinas Medical Center in Charlotte, NC.
p>Dr. Gleaton is passionate about women, youth, and mentoring. She is a Scrubs Camp instructor, a program to increase student entry in healthcare, and serves as a Compassion International adoptive parent. She is also a member of the American College of Obstetrics & Gynecology, the American Association of Gynecologic Laparoscopists, and the American Association of Professional Women.
Sources:
- Kruszyńska A, Słowińska-Srzednicka J. Anti-Müllerian hormone (AMH) as a good predictor of time of menopause. Przegla̜d Menopauzalny = Menopause Review. 2017;16(2):47-50. doi: https://doi.org/10.5114/pm.2017.68591
- Zarek SM, Mitchell EG, Sjaarda LA, et al. Is Anti-Müllerian Hormone Associated With Fecundability? Findings From the EAGeR Trial. 2015;100(11):4215-4221. doi: https://doi.org/10.1210/jc.2015-2474
- Ledger WL. Clinical Utility of Measurement of Anti-Müllerian Hormone in Reproductive Endocrinology. The Journal of Clinical Endocrinology & Metabolism. 2010;95(12):5144-5154. doi: https://doi.org/10.1210/jc.2010-0701
- Toner JP, Seifer DB. Why we may abandon basal follicle-stimulating hormone testing: a sea change in determining ovarian reserve using antimüllerian hormone. Fertility and Sterility. 2013;99(7):1825-1830. doi: https://doi.org/10.1016/j.fertnstert.2013.03.001
- Iliodromiti S, Kelsey TW, Wu O, Anderson RA, Nelson SM. The predictive accuracy of anti-Müllerian hormone for live birth after assisted conception: a systematic review and meta-analysis of the literature. Human Reproduction Update. 2014;20(4):560-570. doi: https://doi.org/10.1093/humupd/dmu003
- Ludmila Barbakadze, J. Kristesashvili, Khonelidze Nl, Tsagareishvili G. The correlations of anti-mullerian hormone, follicle-stimulating hormone and antral follicle count in different age groups of infertile women. 2015;8(4):393-398. doi: https://doi.org/10.22074/ijfs.2015.4179
- Olooto W, Amballi AA, Banjo TA. A Review of Female Infertility; Important Etiological Factors and Management. Journal of Microbiology and Biotechnology Research; 2012. Accessed January 29, 2024. https://www.researchgate.net/profile/Wasiu-Olooto/publication/273322572_A_review_of_Female_Infertility_important_etiological_factors_and_management/links/54febb060cf2eaf210b3bbdd/A-review-of-Female-Infertility-important-etiological-factors-and-management.pdf
Reach Out, We're Here
Have questions about your order or products? For the speediest answer, check out our FAQ section. Need something else? Come find us below.
Please keep in mind our regular business hours; Monday-Friday, 9am-5pm CT.
Customer Support
support@natalist.com
Press Inquiries
media@everlyhealth.com
Business & Partnerships
team@natalist.com
Affiliates + Influencers
team@natalist.com
Job Openings
Careers Page
























